A Practical Guide to Sleeping Through the Night Without Frequent Awakenings
Outline:
– Why uninterrupted sleep matters and what breaks it
– Evening routine and bedroom setup that support continuous sleep
– What to eat and drink (and when) to reduce awakenings
– Calming a busy mind: mental strategies and wind‑down rituals
– Putting it all together: a one‑week plan and knowing when to seek help
Introduction:
You are not alone if your nights feel like a string of interruptions stitched together by the alarm clock. Unplanned awakenings fragment the restorative stages of sleep, trimming memory consolidation, mood stability, and metabolic balance. Adults generally need 7–9 hours, and continuity matters as much as total time. The good news is that most nocturnal awakenings trace back to modifiable habits, environment, or manageable health factors. In the pages ahead, you’ll find practical guidance grounded in sleep science and everyday constraints. Think of it as a calm companion: less perfection, more progress, and a focus on routines you can sustain.
Understanding Night Awakenings: Sleep Architecture, Body Rhythms, and Common Triggers
Before changing your routine, it helps to know what you’re optimizing. Sleep unfolds in cycles of roughly 90 minutes, moving through light sleep, deep slow‑wave sleep, and REM. Brief awakenings often occur at the edges of these cycles; most pass unnoticed. Problems arise when small disruptions—light leakage, noise spikes, temperature swings, mental chatter, reflux, or a full bladder—turn these normal micro‑arousals into full wakefulness. Hormonal patterns also play a role: melatonin rises in darkness to cue sleep, while cortisol typically dips overnight and rises before dawn to prepare you for waking. When these rhythms are bumped by irregular schedules or late‑night light, the night can feel choppy rather than continuous.
Consider the most frequent culprits, which tend to cluster. – Light: Even dim exposure at night can suppress melatonin and increase alerting signals. – Noise: Intermittent sounds (sirens, a neighbor’s door) wake people more than steady background sound. – Temperature: Bedrooms that are too warm increase arousals; many sleepers fare better around 17–19°C (63–67°F). – Substances: Caffeine’s half‑life is about 5–6 hours, and alcohol may hasten sleep onset but fragments the second half of the night. – Stress: Rumination ramps up sympathetic activity, nudging you awake at cycle transitions. – Physiology: Congestion, reflux, restless legs, and sleep apnea disturb continuity and merit attention.
There’s a useful mindset shift: aim to lower the “probability of full wakefulness” at each cycle boundary. You may not control every variable, but reducing total load across light, sound, heat, and internal activation often pays outsize dividends. People sometimes expect one silver bullet; in practice, two or three small improvements combined—earlier light exposure, cooler room, and a steady wind‑down—outperform any single tweak. Over the next sections, you’ll learn how to stack these marginal gains without turning sleep into a second job.
Designing Evenings and Bedrooms That Protect Continuous Sleep
Consistency cues the brain. A stable sleep window anchors circadian timing, making awakenings less likely. Pick a rise time you can honor seven days a week; let bedtime adjust gradually as your body lines up. Morning light is a powerful lever—exposure soon after waking helps set the internal clock so melatonin arrives on time at night. At the other end of the day, dimming household lights about two hours before bed reduces alerting signals. If screens are unavoidable, shift to low‑brightness modes and increase font size to reduce strain rather than relying on late fixes.
Transform the bedroom into a low‑arousal habitat. Fabrics that breathe, a supportive pillow that keeps the neck neutral, and clutter‑free surfaces can matter more than costly upgrades. Consider: – Temperature: Aim for cool air and warm covers so your skin can shed heat. – Light control: Blackout curtains or snug shades reduce early‑morning awakenings from dawn light. – Sound: Steady “masking” noise (white or pink noise) can blunt intermittent sounds that otherwise spike arousal. – Scent and ritual: A familiar, mild scent and a short, repeatable pre‑sleep routine cue the brain that nothing novel is happening, which lowers vigilance.
Wind‑down should be simple, predictable, and genuinely pleasant. Many people benefit from a 30–60 minute ramp that includes quiet reading, light stretching, or a warm shower. Imagine this as a dim hallway leading to sleep rather than a checklist. Keep the bed for sleep and intimacy only; relocating wakeful activities trains the brain to associate the mattress with rest, not struggle. If you awaken and can’t drift back within about 15–20 minutes, step out to a low‑light room for a calming activity until drowsiness returns—this avoids reconditioning the bed as a “wakefulness zone.” Over days, these environmental signals stack, and awakenings lose their grip.
Food, Drink, and Timing: Quieting the Body’s Nighttime Interruptions
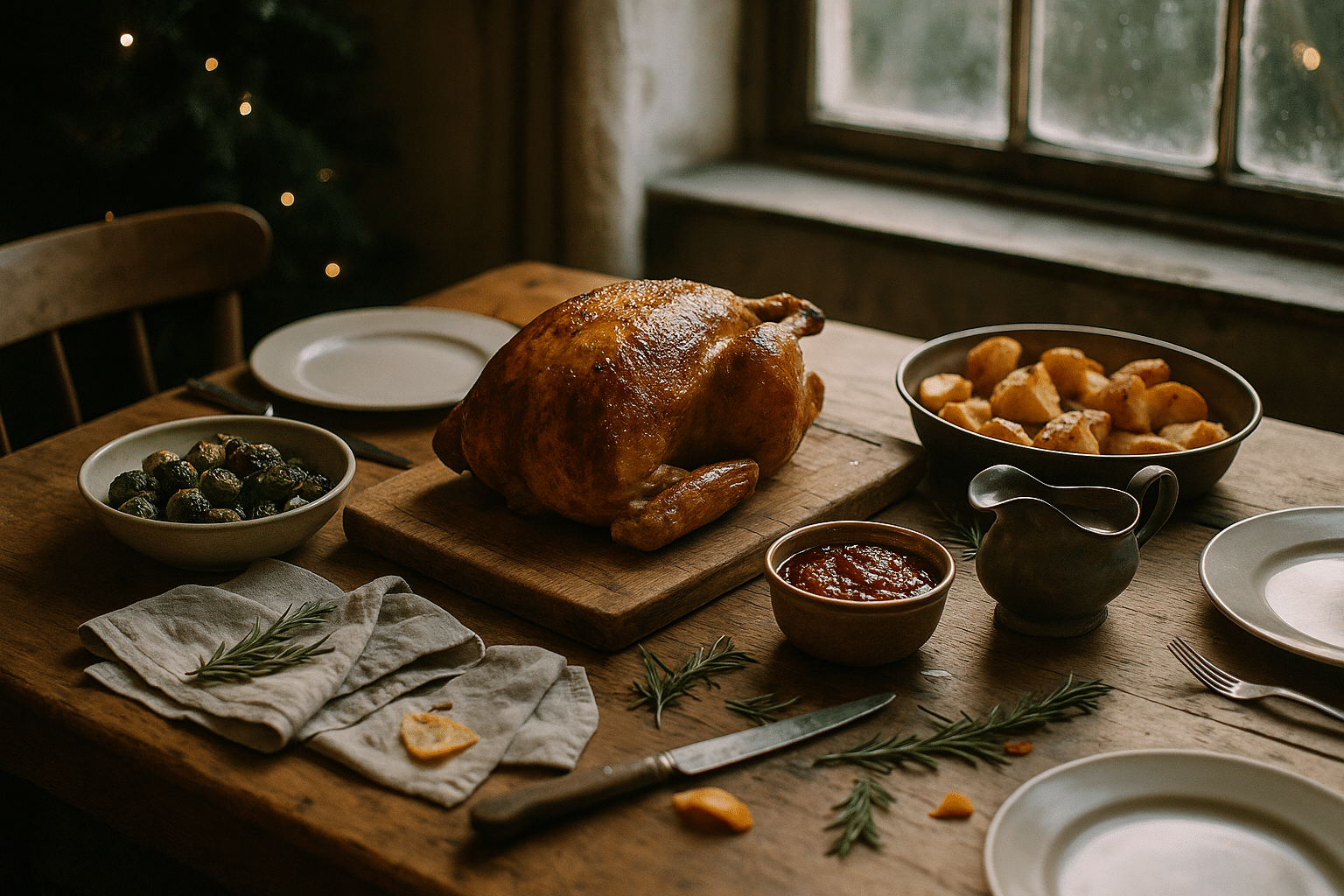
What and when you consume can tilt the odds toward steady sleep. Caffeine is the obvious starting point: with a half‑life around 5–6 hours (and a longer tail in some people), a 4 p.m. espresso can keep receptors nudged into the night. A practical heuristic is to front‑load caffeine to the morning and make early‑afternoon your cutoff. Nicotine is stimulatory as well; evening use often shortens sleep and increases awakenings. Alcohol deserves special attention: it may speed sleep onset, but it suppresses REM early and triggers rebound wakefulness later, especially in the second half of the night when the brain tries to restore balance.
Meals interact with sleep more subtly. Large, late dinners can increase core temperature and exacerbate reflux, both linked to awakenings. Many sleepers do well with a lighter evening meal, finishing two to three hours before bed. Protein and fiber support satiety without the heavy heat load of rich, spicy dishes. If nocturnal hunger wakes you, a small, balanced snack can help—think a modest portion pairing protein with complex carbs to prevent a glucose dip. Hydration follows the “early and often” rule: drink throughout the day and taper in the evening to reduce bathroom trips without courting thirst.
Pay attention to individual sensitivities. – Reflux: Elevating the head of the bed slightly and avoiding late acidic or high‑fat foods can reduce nocturnal symptoms. – Bladder triggers: For some, evening carbonated drinks, citrus, or artificial sweeteners increase nighttime urgency. – Supplements: Magnesium glycinate and glycine are well‑tolerated for many, but effects vary; introduce one change at a time and give it a week to judge. – Temperature: Warm showers 60–90 minutes before bed can promote heat loss afterward, easing sleep onset and potentially reducing awakenings.
Think in terms of gentle guardrails rather than strict rules. A steady morning meal time, front‑loaded fluids, and an earlier dinner build momentum for the night to follow. When life bends the plan—late social meals, travel, or deadlines—compensate by reinforcing other cues (dim light, cooler room, quiet reading). Sleep responds to patterns, not perfection.
Calming a Busy Mind: Cognitive and Behavioral Strategies That Reduce Waking
Many awakenings are mental, not mechanical. You reach a light stage of sleep, open your eyes, and a thought hooks you: the meeting tomorrow, a vague worry, an old memory. The aim is not to banish thoughts but to lower their “stickiness.” Cognitive and behavioral strategies used in structured sleep programs translate well to home practice. Start with a simple rule: if you’re awake and alert in bed for around 15–20 minutes, get up to a comfortable, dimly lit spot and do something low‑key until sleepiness returns. This breaks the spiral of clock‑watching and frustration, which otherwise trains the brain to be vigilant in bed.
Give your mind a place to put unfinished business earlier in the evening. A 10‑minute “worry buffer” helps: write out tasks, uncertainties, and the smallest next steps before wind‑down. You are not solving everything; you’re parking it until morning. Pair this with a gentle breathing pattern that reduces physiological arousal. Try: – Extended exhale breathing (inhale 4, exhale 6–8) to nudge the nervous system toward parasympathetic tone. – Box breathing (4‑4‑4‑4) for a steady rhythm. – Progressive muscle relaxation, scanning and softening major muscle groups from toes to forehead. – Anchored attention, such as counting breaths or repeating a neutral phrase, when thoughts loop.
Another lever is stimulus control: reserve the bed for sleep and intimacy so the context consistently signals “off duty.” If you nap, keep it short (10–20 minutes) and earlier in the day to protect nighttime pressure for sleep. Evening media choices also matter. Fast‑paced or emotionally charged content can echo back at 2 a.m.; swapping to slower‑paced reading or quiet audio reduces residual arousal. Mindfulness can help you notice awakenings without panic—observe, label (“thinking,” “planning”), and return to breath. Over time, these practices shrink the gap between waking and sleep reentry, making nighttime awakenings less eventful and less frequent.
Putting It All Together: A One‑Week Plan, Tracking Wisely, and When to Seek Help
Change lands better when it’s paced. Here’s a realistic week that builds continuity without turning life upside down. – Day 1: Fix your rise time and get 15–30 minutes of outdoor light within an hour of waking. In the evening, dim household lights two hours before bed. – Day 2: Cool the bedroom and simplify bedding. Add a brief wind‑down with light stretching and quiet reading. – Day 3: Move caffeine to morning only; set an early cutoff for alcohol this week. – Day 4: Create a 10‑minute worry buffer and pick one breathing practice. – Day 5: Adjust dinner timing to finish two to three hours before bed; taper fluids after that. – Day 6: Practice the “get out of bed” rule for any prolonged wakefulness. – Day 7: Review what helped and choose two anchors to keep.
Track lightly. A simple sleep diary—bedtime, time to fall asleep, number of awakenings, rise time, and how you feel in the morning—often outperforms gadget readouts for guiding change. If you use a wearable, treat its numbers as rough trends rather than verdicts. Look for patterns: does a late workout correlate with 3 a.m. wakeups, or does morning light shrink them? Keep adjustments small and give each at least several nights before judging; sleep systems adapt gradually.
Know when to ask for help. Nightly snoring with gasps, waking unrefreshed despite long hours, morning headaches, or bed‑partner reports of pauses in breathing suggest sleep‑disordered breathing. Persistent leg urges at night, burning or crawling sensations that ease with movement, point toward restless legs or periodic limb movements. Chronic reflux, chronic pain, thyroid issues, perimenopausal symptoms, and certain medications can all fragment sleep. If awakenings persist for more than a few weeks despite consistent changes, consult a clinician; targeted evaluation and therapies can be transformative. Think of medical input not as a last resort but as a sensible ally when home strategies plateau.
Most importantly, be kind to the process. Not every night will be perfect, and that’s okay. The goal is fewer, shorter awakenings on average, and steadier days that follow. By stacking small cues—predictable light, cool quiet spaces, thoughtful timing of food and drink, and calm mental routines—you create a night that asks less of you. The payoff is subtle but meaningful: mornings that feel like a beginning rather than a recovery.